A doctor monitoring the progress of a patient. PHOTO/PEXELS
By PATRICK MAYOYO
An artificial intelligence (AI) tool accurately predicted which patients would need a skilled nursing facility after leaving the hospital, a new study shows.
Led by researchers from New York University (NYU) Langone Health, the study suggests that quickly identifying these patients would help hospitals plan earlier for complex care and avert stressful situations where patients are medically ready to leave the hospital but have no safe place to go, say the study authors.
Published online recently in the Nature-family journal npj Health Systems, the work found that a model using short, AI-generated summaries of doctor notes was more accurate than models using the original, lengthy doctor notes. This new method uses one AI tool to summarize key risk factors from notes taken by a doctor as a patient is admitted, and a second AI component to predict with 88 percent accuracy the need for skilled nursing care as inpatient hospitalizations end.
“Our two-step approach acts like a fast, careful reader, turning a complex medical note into a simple summary of what matters most for discharge planning,” says senior study author Yindalon Aphinyanaphongs, MD, PhD, director of operational data science and machine learning for NYU Langone, and a research professor in the Departments of Population Health and Medicine at NYU Grossman School of Medicine.
The study addresses skilled nursing facilities, which provide short-term, intensive care and rehabilitation services for patients recovering from an illness or surgery. According to the authors, about 15 percent of patients from NYU Langone are discharged to skilled nursing facilities.
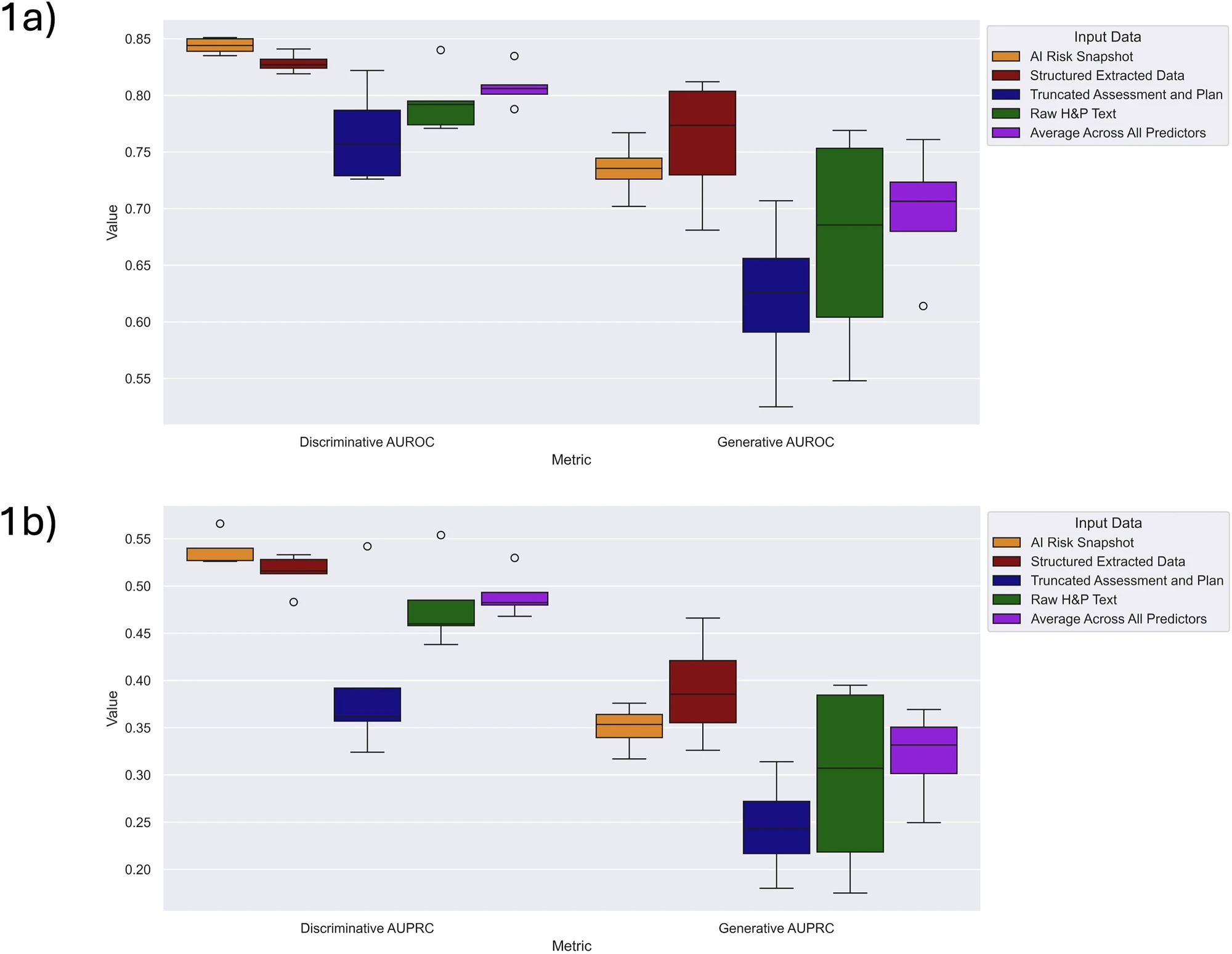
Fig. 1a, b, Supplementary Fig. 1a–i). ELC-derived predictors (AI Risk Snapshot and Structured Extracted Data) resulted in improved average performance on AUROC and AUPRC for discriminative and generative models. IMAGE/ NYU Langone Health.
The research team analyzed the electronic health records of 4,000 patients admitted to general medicine services at NYU Langone. They focused on the “history and physical” admission notes that contain data about a patient’s health, functional ability, and social situation.
Specifically, the researchers developed a generative AI model that reads each lengthy admission note and extracts information related to seven risk factors, such as a patient’s living situation and ability to perform daily tasks, organized into a short “AI Risk Snapshot.”
Finally, the researchers tested nine different AI models to see which could best predict a patient’s discharge destination. They compared the performance of models using the full, raw notes against the models’ snapshots, which were 94 percent shorter than the original notes. This was critical, the researchers say, as nearly all the original, full-length notes were too long for the AI models to process.
To ensure that the AI’s reasoning was sound, the researchers tested its outputs with human experts. When nurse case managers reviewed the AI-generated summaries without seeing the model’s prediction, their assessments strongly aligned with the AI’s risk scores. In fact, a high-risk score from the model made it 13.5 times more likely that a nurse would independently flag the patient as needing skilled nursing care.
“Our next step is to test this model in a real-world clinical setting to see if it helps our care teams plan discharges more effectively across all patients,” says first author William R. Small, MD, a clinical assistant professor in the Department of Medicine. “We will also monitor the system to ensure it is fair and safe and helps to improve patient care.”


